Chronological development
Table 1: Chronology of medical system development in Singapore
| Century / Year | Historical milestone |
| Early settler | Singaporean practised their own traditional folk medicine[i]. |
| 19th century | The first doctor western-trained arrived treated the East India Company officials exclusively[1]. |
| 1844 | A leprosarium built at Pearl’s Hill[1]. |
| 1905 | College of Medicine was founded[1]. |
| 1909 | Tan Tock Seng Hospital was built followed by the municipal hospital known as Municipal Hospital[1]. |
| After the first world war | The period that most of the existing hospitals in Singapore were built1 Outram Road General Hospitals (now Singapore General Hospital) were completed in 1926 Trafalgar Home, the leprosy hospital, were completed in 1926 The Mental Hospital in 1927 – renamed Woodbridge Hospitals in 1951 Kandang Kerbau Maternity Hospitals in 1928 |
| 1921 | Training of public health personnel to deal with the control of infectious diseases and the inspection of food premises, markets, and the other public places were undertaken[1]. |
| 1994 | The Minister of Health appointed a committee on Traditional Chinese Medicine (TCM) to review the practice of TCM and recommend measures to safeguard patient interest and safety, and to enhance the standard of training of TCM practitioners[ii]. |
| 1995 | The committee submitted a report on TCM to the Minister of Health and recommended a phased approach to the regulation of TCM based on the following principles[iii]: A Traditional Chinese Medicine (TCM) Unit was set up in MOH (which was subsequently renamed TCM Department) to coordinate implementation of the committee’s recommendations[iv]. self regulation of TCM practitioners by the TCM community initially followed at a larger stage by statutory regulation upgrade the standard of training of TCM practitioners control of Chinese medicinal materials |
| 1996 | As part of self regulation of TCM practitioners, the following committees were formed to represent the local TCM community in Singapore[3]: Singapore TCM Organisations Coordinating Committee (STCMOCC) to represent the TCM practitioners. Singapore TCM Organisations Committee (STOC) to represent the TCM traders Chinese Proprietary Medicines (CPM) Unit was set up[v]. |
| 1998 | CPM product regulation was gazetted under Medicines Act[vi]. |
| 1999 | With effect from 1 Sep 1999, CPM product regulation was implemented to promote safety and quality of CPM products available in the Singapore market. |
| 2000 | TCM Practitioners Act was passed in 14 Nov 2000 by the parliament[vii],[viii]. |
| 2001 | The Traditional Chinese Medicine Department in MOH was renamed the Traditional & Complementary Medicine Branch. Formation of Traditional Chinese Medicine Practitioner Board (TCMPB)[6]. TCMPB is responsible to register both acupuncturists and TCM physicians; to accredit TCM training institutions and TCM courses for the purpose of registration; and to determine and regulate the conduct and ethics of registered TCM practitioners[ix]. Registration of TCM practitioners in phases. First to be registered: Acupuncturist[6],[8]. |
| 2002 | Registration of TCM Physician started[6],[8]. |
| 2004 | From 1 January 2004, practitioners who wish to practise TCM in Singapore are eligible for registration once they posses[6]: TCM qualifications approved by the TCM Practitioners Board, and Pass the Singapore TCM Physicians Registration Examination (STRE). |
| 2005 | The Transmissible Spongiform Encephalopathy (TSE) Guidelines for Minimizing The Risk of Contamination in Chinese Proprietary Medicines, Traditional Medicines & Health Supplements was issued[5]. Co-located TCM clinics in hospitals operating as a separate entity allowed to provide acupuncture and other TCM services. |
| 2006 | The Ethical Code and Ethical Guidelines for TCM Practitioners were published by the TCM Practitioners Board[6]. The Singapore College of TCM started a Graduate Diploma in Acupuncture Course, conducted in English, to train registered medical and dental practitioners in acupuncture. Graduates of the course who pass the Singapore Acupuncturists Registration Examination (SARE) can be registered as acupuncturists by the TCM Practitioners Board. Voluntary listing of Chinese medicinal materials (CMM) dispensers (i.e. TCM pharmacists). |
| 2007 | Guidelines were revised to allow hospitals and nursing homes to provide acupuncture services as part of their package of medical services to patients. At present in Singapore, western medicine is the core medicinal system being utilized[5],[6]. Nonetheless, it is common practice among the various ethnic groups to consult traditional practitioners for general ailments[11]. Traditional medicine comprising the following historical healing methods still enjoys considerable popularity[13]: |
At present in Singapore, western medicine is the core medicinal system being utilized[5],[6],[i].Current practice
- Nonetheless, it is common practice among the various ethnic groups to consult traditional practitioners for general ailments[11].
- Traditional medicine comprising the following historical healing methods still enjoys considerable popularity[13]:
- Traditional Chinese medicine (TCM) using acupuncture and Chinese medicinal materials (CMM or zhongyao) mainly from China;
- Traditional Malay medicine using Malay medicinal materials (or jamu) mainly from Indonesia and Malaysia; and
- Traditional Indian medicine using Indian medicinal materials (or ayurveda) mainly from India.
- TCM products are Chinese Medicinal Materials (CMM) that include Chinese herbs and medicinal materials obtained from animal and mineral sources used in the practice of TCM. They are grouped as follows[2],[ii]:
- Raw CMM: CMM in natural states or undergone simple processing (e.g. cutting, drying etc.).
- Chinese Proprietary Medicines (CPM): CMM preparations in final dosage forms (e.g. tablets, pills, liquid preparations etc.).
Prevalence
- The survey in 2004, conducted by National University of Singapore, supported that Traditional Chinese Medicine (TCM) is the most frequently utilized Traditional Medicine (TM) by Singaporean followed by the Traditional Malay Medicine (jamu) and Traditional Indian medicine[i] .
Table: Popularity of different forms of CAM
| No. | Modality | Percentage |
| 1 | Traditional Chinese Medicine | 88% |
| 2 | Traditional Malay Medicine | 8% |
| 3 | Traditional Indian Medicine | 3% |
| 4 | Other forms of CAM | 1% |
| TOTAL | 100% |
Table constructed based on information from: Lim, M. K. et al. Complementary and alternative medicine use in multiracial Singapore. Journal Complementary Therapies in Medicine, 2005.
- It also exhibited that gender and ethnicity were important in determining factors that affect the utilization of TM/CAM. It showed that among the ethnic, 84% Chinese were using the TM/CAM, with Malay and Indian at 69% respectively[ii].
Administration
Official Body
Contact Address :
Traditional & Complementary Medicine Branch
Ministry of Health, College of Medicine Building
16 College Road
Singapore 169854
Contact No. : (65) 6325 9220
Fax No : (65) 6235 9499
Email : [email protected]
Website : www.moh.gov.sg
Main therapies
- In Singapore, Traditional Chinese Medicine is the most popular form of Traditional and Complementary Medicine[6].
- Traditional Malay Medicine and Traditional Indian Medicine are also available as are ‘Western’ Complementary and Alternative Medicine (CAM) modalities such as aromatherapy and chiropractic[13].
Policy & Regulations
- Regulation
- The TCM Practitioners Board oversees the regulation of TCM practice[9].
- The Health Sciences Authority (HSA) is the authorised body in charge of health product regulation. The Complementary Health Products Branch of HSA oversees the regulation of Chinese Proprietary Medicines (CPM), other Traditional Medicines and Health Supplements[5],[6].
- Policy
- The Singapore’s National Policy on Traditional/Complementary Medicine was issued in 1995[13].
- The policy proposed[3],[13]:
- A phased line attempt to TCM regulation
- Promote standard of TCM training
- Control of Chinese medicinal materials
- Act
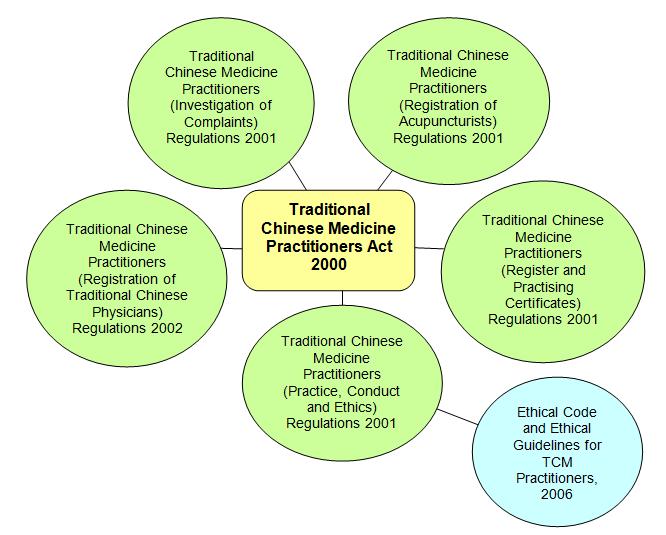
- The Singapore Parliament passed The Traditional Chinese Medicine Practitioners Act on 14 Nov 20006,[7],[8],[11], [13].
- The Act requires TCM practitioners who undertake the prescribed practice of TCM to be registered with the TCM Practitioners Board[8].
- Legislations regulating TCM Practice:
- Legislations regulating CPM products:
- The Medicines Act
- The Poisons Act
- The Sale of Drugs Act
- The Medicines (Advertisement and Sale) Act
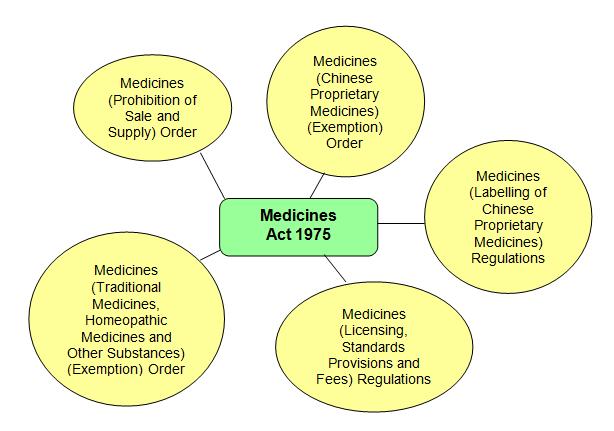
Chinese Proprietary Medicines (CPM) regulation requires the local dealers to obtain the appropriate licences before they can import, wholesale, manufacture or assemble CPM. All CPM products must meet stipulated safety and quality criteria before they can be approved by the HSA [5],[8].
Unlike CPM, it is currently not necessary for other traditional medicines and homeopathic medicines to obtain approvals from HSA. The accountability of safety and quality of these products lies with the dealers and sellers. They must comply with legal requirements, such as the absence of legally prohibited substances, limits of toxic heavy metals and prohibition of legally stipulated strong medical claims e.g. cancer, diabetes.
An advertising permit is also required for advertisement and promotional activities for CPM and traditional medicines.
In addition to the pre-marketing activities, HSA carries out post-marketing surveillance activities to ensure timely detection and the removal of any unsafe products from the market. These surveillance activities include:
- Adverse reaction reporting;
- Testing of products sampled from the retail market using a risk-based approach;
- Intelligence gathering including investigation of feedback from members of the public and the media
- Information exchange with other national authorities.
Facilities
Settings
- In the past, the use of acupuncture was allowed on clinical research basis in several hospitals[7];
- Ang Mo Kio Community Hospital
- National University Hospital
- Singapore General Hospital
- Tan Tock Seng Hospital
- Today, the Singapore government allows acupuncture as well as other TCM services (e.g. Chinese herbal medicine and Chinese therapeutic massage ‘Tuina’) to be offered in hospitals and nursing homes. However, such services are only allowed on an outpatient basis and provided by a TCM clinic co-located within the premises of the healthcare institutions as a separate entity (except for acupuncture services which could be provided by the healthcare institutions as part of their medical services to their patients, and inpatients would be allowed to seek acupuncture treatment with a doctor’s referral)[8].
- In addition, registered medical and dental practitioners (who are also registered acupuncturists/TCM practitioners) are allowed to provide acupuncture services as part of their package of services to their patients in their medical clinics[8].
- Hospitals and medical centres that have a co-located TCM clinic within their premises include:
- Singapore General Hospital
- Institute of Mental Health
- Khoo Teck Puat Hospital
- Raffles Hospital
- Thomson Medical Centre
- Ren Ci Community Hospital
- Hospitals that provide acupuncture as part of their medical services to patients include:
- Singapore General Hospital
- Tan Tock Seng Hospital
- National University Hospital
Research Institute
- In 1995, an Acupuncture Research Clinic was set up by the Singapore Ministry of Health at the Ang Mo Kio Community Hospital[3]. The hospital has been renamed as Ang Mo Kio – Thye Hua Kwan Hospital and now runs a TCM clinic offering TCM services as a supplement to its step-down and rehabilitative care plan.
- Other institutions that have carried out TCM research are:
- National University of Singapore
- Nanyang Technological University
- Singapore General Hospital
- National University Singapore
- Tan Tock Seng Hospital
- KK Women’s and Children’s Hospital
- The Health Sciences Authority
- The National Cancer Centre
- Research projects conducted include use of TCM and acupuncture in pain control, stroke rehabilitation and smoking cessation.
Training & Education
In 2002, Singapore Ministry of Health worked with the local CMM community to conduct a formal training course in CMM herbal dispensing jointly with China’s Beijing University of Chinese Medicine. Graduates of the course have been listed voluntarily with the TCM Practitioners Board in preparation for future registration of this group of practitioners.
Presently, there are four local institutions accredited by the TCM Practitioners Board to provide TCM training courses:
- Nanyang Technological University
- Singapore College of Traditional Chinese Medicine
- Institute of Chinese Medical Studies
- TCM College
| Training Institution | TCM Courses |
| Nanyang Technological University | Double Bachelor degrees programme, ( 5-year full time) with the Bachelor degree in Biomedical Sciences awarded by Nanyang Technological University and the Bachelor degree in Chinese Medicine awarded by Beijing University of Chinese Medicine. |
| Singapore College of Traditional Chinese Medicine | TCM Bachelor degree courses (5-year full time or 7-year part time), jointly conducted with Guangzhou University of Chinese Medicine. Master degree programme in TCM (3 year) jointly conducted with Nanjing University of Chinese Medicine. Doctor degree programme in TCM (3 year) jointly conducted with Nanjing University of Chinese Medicine. Graduate diploma in acupuncture course (405 hours part-time course conducted in English and only for Singapore registered medical or dental practitioners) |
| Institute of Chinese Medical Studies | TCM Bachelor degree course (7-year part time), jointly conducted with Beijing University of Chinese Medicine. Master degree programme in TCM (3 year), jointly conducted with Beijing University of Chinese Medicine. |
| TCM College | CMM training courses: Elementary programme (2- year part time) Intermediate programme (1½ -year part time) Diploma course in Chinese Medicine Pharmacy (1-year part time) |
Links
Singapore Ministry of Health: http://www.moh.gov.sg
Traditional Chinese Medicines Practitioners Board: http://www.tcmpb.gov.sg
Health Sciences Authority: http://www.hsa.gov.sg
References
- Singapore Ministry of Health (1975). Singapore 1975. Ministry of Health. Singapore.
- Singapore Ministry of Health. Traditional Chinese Medicine. The Report by the Committee on Traditional Chinese Medicine (Oct 1995). Retrieved from http://www.gov.sg/moh/mohiss/tcm/tcmrpt.html
- Country Report for ASEAN Ad-hoc Working Group Meeting on Traditional & Complementary Medicine (AWGTCM) on 17 April 2004 in Penang, Malaysia
- World Health Organization (2005). National Policy on Traditional Medicine and Regulation of Herbal Medicine. Report of a WHO Global Survey. WHO. 2005. Page : 137
- Health Sciences Authority. Retrieved from http://www.hsa.gov.sg Accessed 21 July 2008
- Heng C. H. The Regulation of Traditional Chinese Medicine in Singapore. Presented at the 2006 Government Forum on Traditional Medicine (2006GFTRM), Beijing, 26 – 27 Oct 2006.
- Lee, T. L. (2006). Complementary and Alternative Medicine, and Traditional Chinese Medicine : Time for Critical Engagement. Retrieved from www.annals.edu.sg/PDF/35VolNo11Nov2006/V35N11 p749.pdf. Accessed 2 July 2008.
- Ministry of Health Singapore. Retrieved from http://www.moh.gov.sg/mohcorp/hcsystem.aspx?id. Accessed 1 Ogos 2007.
- Traditional Chinese Medicine Practitioners Board. Retrieved from http://www.tcmpb.gov.sg/tcm/index.jsp 31 July 2007.
- Singapore Chinese Physicians’ Association. Retrieved from http://www.singaporetcm.com/eng/index.html. Accessed 13 Jun 2008
- World Health Organization (2001). Legal Status of Traditional Medicine and Complementary/Alternative Medicine: A Worldwide Review. World Health Organization.
- Presentation Dr. Cheah C., in Integrating Traditional and Complementary Medicine into the National Healthcare-Singapore’s Experience.
- Lim, M. K., Sdarangani, P., Chan, H.L., Heng, J.Y. (2005). Complementary and Alternative Medicine Use in Multiracial Singapore. Complementary Therapies in Medicine;13:16-24
- Ministerial Advisory Committee on Complementary and Alternative Health, Ministry of Health (2003). Complementary and Alternative Medicine. Current Policies and Policy Issues in New Zealand and Selected Countries. A discussion document 2003. Ministry of Health. New Zealand.

