
Global Information Hub on Integrated Medicine.2016.pg 1-28.
Meor Hakimi Meor Idris , Ida Farah Ahmad , Mohd Khairuddin Che Ibrahim, Siti Nurulsyuhada Rosli, Nurul Nadhirah Abdul Razak, Farhanah Ramawi, Nur Hazwani Norhata, Ami Fazlin Syed Mohamed
Information Unit, Herbal Medicine Research Centre, Institute for Medical Research, Jalan Pahang, 50588 Kuala Lumpur
ABSTRACT
Background
For the past few years, flaviviral infection, mainly dengue fever, causes a large number of morbidity and mortality in Malaysia. There was an 18.1% increase in the number of dengue cases nationwide with 68% increase in mortality, compared to previous year. 8-Hydroxyquinoline, derived from the bark of Cinchona tree has the potential antiviral property to inhibit dengue viral replication.
Objectives
To conduct a review on published articles on the effectiveness of 8-Hydroxyquinoline derivatives in treating dengue fever, as well as to review its activity based on its molecular structure.
Methodology
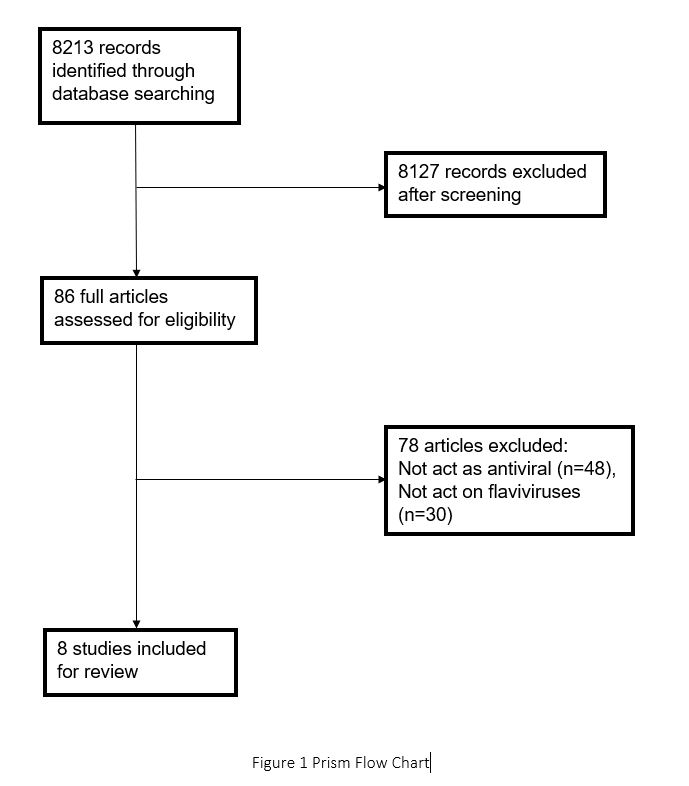
A comprehensive database search was done in February till April 2015 involving PubMed, Wiley, Scopus, EbscoHost, ScienceDirect, SpringerLink, OVID, and Nature using 6 keywords combination. The database search showed 8213 records and 8 articles were included for full review.
Main Results
Only in vitro experiments were available at the moment the review was conducted. Out of the 8 papers, 6 were experiments about 8-Hydroxyquinoline tested on dengue virus, West Nile virus, and few other pathogens. 2 were review papers discussing the potential antiviral drug target based on the molecular structure of flavivirus. The compounds has 8-Hydroxyquinoline scaffold at R1 with different derivatives at R2 and R3, except for Amodiaquine which is a 4-aminoquinoline. The compounds bind to the active site of NS2B/NS3 protease in a competitive manner, except for Amodiaquine which may act at earlier steps of viral replication. The cytotoxicity levels of each compound varies and some were not well established.
Conclusion
8-Hydroxyquinoline derivatives may have the potential as an antidengue agent with further researches put into work.
Keywords
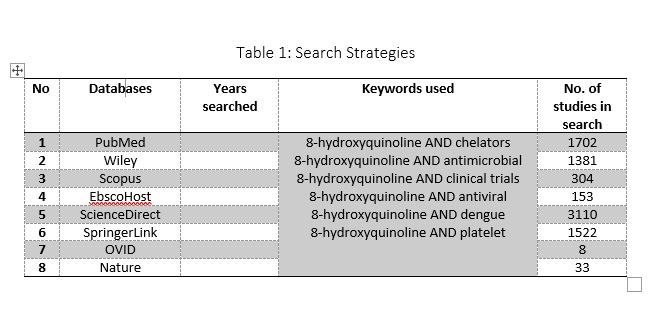
8-hydroxyquinoline AND chelators, 8-hydroxyquinoline AND antimicrobial, 8-hydroxyquinoline AND clinical trials, 8-hydroxyquinoline AND antiviral, 8-hydroxyquinoline AND dengue and 8-hydroxyquinoline AND platelet
INTRODUCTION
Dengue fever is an important arthropod-borne viral infection (1). From 1780 to 1940, the occurrence of dengue fever was scarce however after World War II (1935 – 1945) erupted, the epidemics and symptoms of dengue fever has emerged (2). 125 countries are dengue endemic (3) including Southeast Asia, Western pacific and the Americas (1). It was estimated that 390 million people are infected each year including 500 000 children (4). The symptoms range from mild flu-like illness to more severe, fatal form called dengue haemorrhagic fever (DHF) and dengue shock syndrome (DSS) (5).
The clinical course of dengue fever has three phases; febrile phase, critical phase and recovery phase. The crucial part is the critical phase marked by ongoing vascular permeability which can lead to organ impairment. The standard treatment are fluid resuscitation and supportive care (6). According to Ministry of Health Malaysia, the cumulative cases of dengue fever starting from January up to November 2015 was 104 910. Compared to similar timeframe in 2014, this was an 18.1% increase with 88 806 cases reported. The mortality rate showed 68% increase with 284 death compared to 189 in 2014 (7). Till date, there is no drugs or vaccines available to treat dengue (1). However it is worth noted that two large scales randomized, placebo controlled, phase 2b and phase 3 clinical trials have been conducted in Thailand and five Asia Pacific countries in 2012 and 2014, respectively, using a recombinant, live-attenuated CYD tetravalent dengue vaccine in healthy schoolchildren have shown 30.2% (95% CI -13.4 – 56.6) and 56.5% (95% CI 43.8 – 66.4) efficacy, respectively, with good safety profile (8, 9).
1.2 Dengue virus and NS2B/NS3 protease
Dengue virus belongs to Flaviviridae family. It has four different serotypes called DENV1-4. The virus is transmitted by Aedes genus of mosquito, particularly Aedes aegypti and Aedes albopictus (8). Other flavivirusare West Nile virus, Japanese encephalitis, and Murray Valley encephalitis virus (9).
The genome structure of flavivirus consists of a positive sense single stranded RNA of 11kb in length encoded into a single polyprotein precursor (10). The polyprotein is translated into 10 mature genes which is made up of three structural proteins (capsid [C], premembrane [prM] or membrane [M], and envelope [E]) and seven nonstructural (NS) proteins namely NS1, NS2A, NS2B, NS3, NS4A, NS4B, NS5. Lai et al (10) stated that the structural proteins form the virion and the nonstructural proteins are manifested in the infected cells and are crucial for viral replication.
The N-terminal of NS3 shows protease activity and this domain interacts with NS2B, a mandatory cofactor needed to form the NS3/NS2B active serine protease complex (11). Brecher et al (11) mentioned that the NS2B/NS3 protease complex is vital in processing the polyprotein precursor leading to release of mature individual nonstructural proteins. This makes the protease complex the prime target for the development of potential antiviral therapy (11).
1.3 Quinoline, the Cinchona alkaloid
Quina quina is a common name for Cinchona bark (12). The Cinchona sp. belongs to Rubiaceae family (12). Globinmed described “the term ‘Cinchona’ refers to several species that cross-breed creating hybrids that are difficult to specifically classify” (13). Species included in the genus Cinchona among others are, Cinchona officinalis L., Cinchona calisaya Wedd., Cinchona antioquiae L. Andersson, and Cinchona asperifolia Wedd. (14). The other common names are Quinine bark, quina, quinine, kinakina, China bark, cinchona bark, yellow cinchona, red cinchona, Peruvian bark, Jesuit’s bark, quina-quina, calisaya bark, fever tree (12). This plant is native to South America, mainly Ecuador but is also found in Bolivia, Costa Rica, Peru and Venezuela (13). The name of the tree was named after the Countess of Chinchon in Peru, who was thought recovered from a fever by using the bark of the tree (15).
The most used part is the bark and wood. It was traditionally used as digestive tonic, to treat malaria, arrhythmias, nocturnal leg cramps and intestinal parasites (13). A typical Cinchona bark contains about 16% quinoline alkaloids. The alkaloids are primarily quinine; the other alkaloids are quinidine, cinchonine, and cinchonamine. Cinchona sp. also contains tannins, bitter triterpenic glycosides also known as quinovin, and quinic acid (13). The Cinchona alkaloids are composed of a hydroxyl group in the centre, with quinoline and quinuclidine rings (16).
Although the bark is the main source of quinoline alkaloids, dimeric alkaloids were not isolated from the bark. A lot of dimeric alkaloids were synthetically manufactured by exploiting several reactive sites of the Cinchona alkaloids (16). Quinoline is the main raw material used in the production of other specialty chemicals. A report in 2005 mentioned that 4 tonnes of quinoline were produced every year (17). It is principally used as the precursor of 8-hydroxyquinoline (17).
Smith (1953) listed seven monohydroxyquinolines and they are divided into two groups by its chemical properties (18). The 3-, 5-, 6-, 7- and 8-Hydroxyquinolines act like phenols while the 2- and 4- derivatives behave as quinolones (19) . Out of the seven, 8-Hydroxyquinoline (8HQ) is the one worth further exploration due to its numerous functions (19).
1.4 8-Hydroxyquinoline (8HQ)
8-Hydroxyquinoline has multifunctional properties (20) and is a potent metal chelator (18) which renders its usefulness for analytical and separation purposes and metal chelation (20). It is widely used as a fungicide in agriculture and a preservative in the wood, textile and paper industries (18). Due to its broad range of biological activities and therapeutic potentials (20), quinoline compounds have been considered good starting materials for the search of novel antimicrobial and antiviral agents.
It has antineurodegenerative, anticancer, antibacterial, antiviral, antitubercular, antiparasitic, antiparasitic, antioxidant and anti-inflammatory properties (20). Its notable antiviral activity in HIV; the synthesis of hydroxyquinoline-polyamine conjugates act as a prototype for antihuman immunodeficiency virus and has reached Phase II clinical trial (22).
1.5 Research objective
The uprising incidence of dengue in Malaysia and a paucity of treatments are major concerns both to the public and the Ministry of Health. This has led interest in drug development targeting dengue virus replication. This review is aiming
- To determine the effectiveness of 8-Hydroxyquinoline in treating dengue.
- To review the activity of 8-Hydroxyquinoline as an anti flaviviral based on its molecular structure.
The second chapter of this review will describe the search strategy, the third chapter outlines the significant findings, the fourth chapter discusses the advantages and disadvantages of the reviewed articles, the firth chapter listed the limitations of the reviewed articles and finally some recommendations on future work.
METHODS
Search strategy
The search to look for related published articles was done using eight electronic databases with six keywords and combinations (as shown in Table 1). Bird’s eye view strategy was applied to identify all the properties of 8-Hydroxyquinoline and its derivatives. Relevant studies were further identified by going through the citations and lists of references in the related articles. All the related articles found in English were included. Two authors independently conducted the literature search by dividing the list of databases followed by cross-checking to avoid redundancy. The years searched were set as default. The search lasted from February till April 2015. The extensive literature search brought about 8213 published articles. The result is shown in Figure 1.
Selection of Samples and Intervention
Studies using 8-Hydroxyquinoline scaffold with various derivatives tested on dengue virus, West Nile virus, Escherichia coli, Pseudomonas.aeruginosa, Avian paramyxovirus type 1, Laryngotracheitis virus, human immunodeficiency virus type 1 were selected.
Selection of Outcomes
Studies reporting on the ability of 8-Hydroxyquinoline derivatives to inhibit WNV or DENV replication were chosen as well as its ability to inhibit few other pathogens.
Selection of Study Model
Only in vitro experiments were available and included.
Data Extraction
The abstract of the searched articles were screened followed by full text reading for articles fulfilling the inclusion criteria. The inclusion criteria were based on samples, intervention, outcomes and study design. Only articles published in English were reviewed and extracted. Out of 86 full text articles obtained from data searching, only 8 studies met the inclusion criteria and included in the review. Both authors work independently in analysing the 8 studies and tabulate the data into the table as described in Table 2. This is done to reduce bias.
Limitations
The main objective of this review is to study the potential ability of 8-Hydroxyquinoline to treat dengue fever, however due to limited resources, its action on West Nile virus and few other pathogens were included. Both original articles and review papers were included. The keywords and combinations used for data searching did not include West Nile virus and the findings of related articles was coincident. The term platelet and clinical trial were also used in database searching but no relevant papers were found.
RESULTS
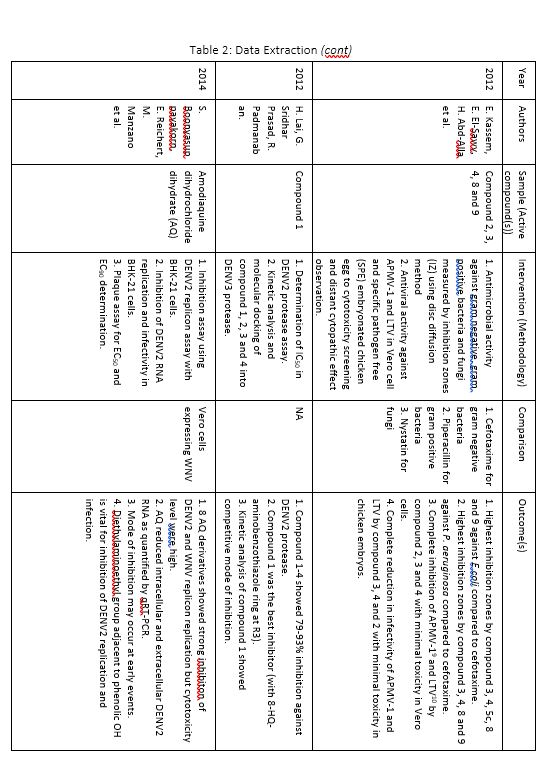
The bird’s eye view search produced 8213 related articles. Out of this, a total of 8 articles were included for full text reading and evaluation (9, 10, 11, 24, 30, 31, 32, 33). 3 papers were written based on laboratory experiments of 8-Hydroxyquinoline on dengue virus (10) and West Nile virus (9, 30). 2 review papers discussed the possibility of developing antiviral therapy based on the molecular structures of flavivirus, but not specific to 8-Hydroxyquinoline (11, 24). These 2 papers served as a useful key knowledge on the quest for antiviral drug development. The other 3 papers were experiments conducted using 8-Hydroxyquinoline derivatives tested on various virus and bacteria (32, 33) comprising one study tested on dengue virus (31).
The studies included were all in vitro experiments. There was no in vivo or clinical trials conducted using 8-Hydroxyquinoline derivatives on dengue patients found during the search exercise. Hereafter, this paper aims to narrate the effectiveness and the activities of 8-Hydroxyquinoline and its derivatives especially in treating dengue fever.
The compounds discovered contained 8-Hydroxyquinoline scaffold (2 aryl substitution at 7-position) at R1 in common with different derivatives at R2 and R3. Compound B (30), compound 14 (9), compound 1 (10) and Amodiaquine (31) showed good potencies in inhibiting and/or WNV and DENV2 proteases with significant values and in a competitive mode of inhibition. Molecular modelling supported that they bind in the substrate-binding cleft and blocked substrate binding to the active site thus inhibit protease activity (9, 10, 30) while Amodiaquine may act at earlier steps in viral replication (31). Most experiments used DENV2 protease assay (10, 30, 31). Compound 2, 3 and 4 showed minimal toxicity (32), compound B exhibited moderate toxicity while compound A exhibited siginificant cytotoxicity (30). The toxicity of Amodiaquine (31), compound 4g and 4i (33) were not well interpreted while the rest of compounds were not tested for cytotoxicity (9, 10).
The studies were carried out in Taiwan[31,32], Hong Kong[33] ,India[34], Hungary[35], South Korea [36] and the United States of America[37]. Sample sizes varied from 28 to 94, with a total of 382 participants aged from 19 and above. Out of seven, only one study reported patients with primary insomnia[33]. The other six studies characterised their participants as having secondary insomnia comprising of volunteers from community services centre[31], selected local areas[32], shelter for abused women[37], a university[35], outpatients with major depressive disorder[34] and inpatients with post-coronary angiography[36].
These studies employed a variety of duration for the music intervention, as well as the frequency and interval between applications. Music duration is at 45 minutes in Chang [33], Deshmukh [34], Harmat [35] and Lai [32], whereas Chan [31], Hernandez-Ruiz [37] and Ryu [36] had the music full duration at 30, 20 and 53 minutes respectively, or let the music on until they fall asleep.. Chan played the music during visits to the participants’ homes once a week for four weeks [31]. The rest of the studies had the participants play the music at bedtime every day [32,35,37] except for Ryu which study was only carried out on a one-time application of the music therapy [36]. However, the number of days and intervals of application also differ between studies. Chang’s was applied for four consecutive days [33], Hernandez-Ruiz for 5 days [37], Lai and Harmat for three weeks [32,35], and Deshmukh for four weeks [34]. Follow-up of the participants were carried out daily by Chang and Hernandez-Ruiz [33,37]. Chan and Harmat had the follow-up once a week [31,35], Deshmukh fortnightly (four follow-up consisted of day-1, day-15, day-30 and day-45) [34] and Lai twice a week [32].
DISCUSSION
The prospect for developing antidengue agent
West Nile viral infection and dengue fever are common infectious diseases however the former is more common in the Western hemisphere (23) . Around the globe, the infections continue to spread as a result of changing climates, growing urbanization and global travel (24).
In the natural course of dengue fever, it was observed that there is a rapid decline in the viral levels (24) down by 10-fold in the first 24 hours and further drop by 100-fold within 48 hours (25). An antidengue therefore must be fast acting and able to decrease the viral burden by more than 10-fold to render it clinically beneficial (24). The large difference in plasma viremia (by more than 10-fold) between non severe dengue fever and severe dengue (DHF/DSS) patients (25) suggested that by reducing the viral load during the early phase of infection may prevent or lower the risk of patients progressing into DHF or DSS (24).
Lim et al listed seven possible approaches in developing antidengue drug. The methods could be by inhibiting the viral entry (entry inhibitors), inhibiting the capsid (C) protein (capsid inhibitors), inhibiting the NS4B (one of the seven nonstructural proteins), inhibiting the protease (protease inhibitors, PIs) inhibiting the C-terminal protein of NS3 protein (helicase inhibitor), inhibiting N-terminal domain of NS5 protein (methytransferase inhibitor) and by inhibiting NS5 polymerase (polymerase nucleoside analog inhibitors) (24).
Directing at viral proteases is a proven strategy as evidenced by the success of developing ten HIV-1 protease inhibitors (PIs) (26) and two HCV (Hepatitis C virus) PIs (27). Hence it is reasonable that a protease inhibitor for DENV would work as efficaciously. This approach is more advantageous in that selecting compounds that mimic or exceed the substrate in affinity for the enzyme would be a sufficient starting point (11). However, this approach has certain drawbacks as well which explained the limited success accomplished so far (11). Brecher et al provided three reasons for this (11).
First, the NS2B/NS3 has a flat, featureless and hydrophilic active site (11). This property, which is similarly found in the development of HCV protease substrate-based inhibitors, makes it difficult for inhibitors to bind tightly to the active site resulting in a low threshold to resistance and extensive cross-resistance (28). Plus, the protease of the four DENV serotypes showed very similar substrate specificity (29). Thus, potential drug resistance should be considered in developing active-site inhibitors for flavivirus protease. Secondly, the NS2B/NS3 active site is similar to host serine proteases in that many compounds are likely to impart toxic effects to the host (11). Thirdly, the active site prefers positively charged moieties which may affect compound bioavailability (11).
The activity and effectiveness 8-Hydroxyquinoline on WNV and DENV
8-Hydroxyquinoline is one of the small molecular inhibitors targeted towards WNV and DENV NS2B/NS3 protease. The three laboratory in vitro experiments included in this section were conducted by various researchers in the United States within 6 years timeframe with chronological pattern observed. Hence the review is written in sequential order.
The first in vitro study identified was by Mueller et al in 2008 (30). Using High-Throughput Screen (HTS) method and fluorogenic tri-peptide substrate, t-butyl-oxycarbonyl (Boc)-Gly-Lys-Arg-7-amino-4-methyl coumarin (AMC), 98 inhibitor compounds were recognised with three different core chemical structures (1-3). Secondary screening discovered two compounds belonging to the 8-Hydroxyquinoline family (compound A and B). Both compounds have core 1, with two aryl substitutions at 7 position of the 8-HQ ring (R1) linked either to –NH-C=O or –NH- group. Analysis for inhibition of both compounds towards WNV and DENV2 proteases in vitro showed significant inhibition of WNV proteases but was 10-fold less effective in the DENV2 protease assay using Boc-Gly-Arg-Arg-AMC substrate. The compounds displayed some selectivity toward WNV protease since the original HTS were done using WNV protease. Also, it is because the amino acid sequences in the carboxy terminal regions of the NS2B cofactor domains were different for the two proteases. This region determined the substrate specificities of the proteases.
Further tests revealed that compound B is less toxic and a more potent WNV RNA replication inhibitor compared to compound A. Compound B inhibited the enzymes in a competitive mode which was substantiated by molecular docking. Compound B had the –NH- group (30).
4 years later Ezgimen et al (9) used 16 8-HQ derivatives including compound B (discovered in the previous study) as a positive control and one additional compound (compound 26) which has naphthalene-1-ol instead of 8-HQ scaffold to determine their percent inhibition of WNV NS2B/NS3pro, to develop structure-activity relationship and mode of inhibition. This study used two fluorogenic substrates; tri-peptide substrate Boc-Gly-Lys-Arg-AMC, similar to previous study; and tetra-peptide substrate Benzoyl (Bz)-norleucine (Nle)-Lys-Arg-Arg-AMC with a different aryl substitutions at R2 and R3.
9 out of 16 compounds with 8-HQ scaffold exhibited inhibitory activity of >95% whereas the rest showed percent inhibition around 20-80%. 14 out of 16 compounds had either aminothiazole or benzaminothiazole ring at R3 and phenylmethyl, phenolic hydroxyl, or benzyloxy phenyl as R2 substitution. Compound 14 was identified as the most potent inhibitor with competitive mode of inhibition. More importantly, SAR revealed N at 1-position of 8-HQ ring was important for WNV protease inhibition because substitution of 8-HQ ring with a naphthalene-1-ol ring (N replaced with –CH-) reduced inhibitory activity by ~75% (decreased from ~99% to 26%) (9).
Lai et al (10) selected derivatives of 8-HQ scaffold that worked on WNV protease and assayed them for inhibition against DENV2 NS2B-NS3pro. Tetra-peptide substrate Benzoyl (Bz)-norleucine (Nle)-Lys-Arg-Arg-AMC was used as Li et al (29) found that it is the optimum substrate for DENV2 protease. The 6 compounds used were from previous study (9) plus a novel compound (compound 1). All have aryl substitution at 7-position with a thiazole or a benzothiazole moiety as an R3 aryl substitution and phenyl, phenylhydroxyl, 2-(benzyloxy)phenyl or 3-(benzyloxy)phenyl moiety as an R2 substitution.
In the DENV2 in vitro protease assay, compound 1 exerted the maximum inhibition, bearing 8-HQ scaffold with two aryl substitutions at 7-position, 3-(benzyloxy)phenyl moiety in the meta position and amino-benzothiazole moiety at R3. It inhibited the DENV2 NS2B-NS3 protease in a competitive manner by competing with substrate binding in the vicinity of the active site which was supported by molecular modelling (10).
Other Quinoline derivatives against DENV2 and different pathogens
Amodiaquine dihydrochloride dihydrate (4-[7-chloroquinolin-4-yl)amino]-2(diethylaminomethyl)phenol) (AQ), a known antimalarial drug containing 4-aminoquinoline was shown to inhibit DENV2 replication and infectivity in a more refined study led by Boonyasuppayakorn using BHK-21 cells/DENV2 replicon cells (31). The reducing levels of intracellular and extracellular DENV2 RNAs as well as extracellular virions quantified by qRT-PCR showed AQ effectively inhibited DENV2 replication. It also inhibited DENV2 infectivity measured by plaque assay with significant EC50 and EC90. The value of CC50 was reported however there was no comparable value. AQ may inhibit early events including translation of viral RNA, events prior to RNA assembly and at the onset of RNA replication. Both p-hydroxyanilino and diethylaminomethyl were crucial moieties for inhibition.
A series of 5-substituted sulphonyl-8-Hydroxyquinoline derivatives were fused with pyranopyrazole and pyranoimidazole resulted in the synthesis of 26 new compounds and tested for antimicrobial (including fungi) and antiviral evaluation (32). Compound 3 (5-(3-Amino-5-oxo-1,2-dihydropyrazol-1-yl)sulphonyl-8-hydroxyquinoline), compound 4 (5-(5-Oxo-1,2-dihydropyrazol-3-yl)sulphonyl-8-hydroxyquinoline), compound 8 (5-(2-Thioximidazolidinon-1-yl)sulphonyl-8-hydroxyquinoline) and compound 9 (5-(2,4-Dioxo-imidazolidin-1-yl)sulphonyl-8-hydroxyquinoline) showed highest growth inhibition zones of Escherichia coli (compared to reference drug cefotaxime) and Pseudomonas aeruginosa (compared to reference drug cefotaxime). The result on fungal inhibition was not mentioned. On the other hand, compound 2 (5-(2-Acetyl-3-amino-5-oxo-1,2-dihydropyrazol-4-yl)sulphonyl-8-hydroxyquinoline), compound 3 and compound 4 exerted complete inhibition of Avian paramyxovirus type 1 (APMV-1) and Laryngotracheitis virus (LTV) in Vero cells and fully reduced their infectivity in the specific pathogen free (SPF) embryonated chicken eggs with substantial therapeutic indices and absence of obvious toxicity.
A preliminary research led by Zeng et al using a series of ten novel 5,5’-(p-phenylenebisazo)-8-Hydroxyquinoline sulfonates were experimented to look for new anti-human immunodeficiency virus type 1 (HIV-1) agents in vitro (33). Compound 4g (5,5’-(p-phenylenebisazo)-8-Hydroxyquinoline p-ethyl-benzenesulfonate) and 4i (5,5’-(p-phenylenebisazo)-8-Hydroxyquinoline p-chlorobenzenesulfonate) displayed more potent anti-HIV-1 activity by reducing its syncytia formation with good therapeutic indices. Preliminary SAR revealed the ethyl group or the chloro atom at 4’-position on the phenyl ring was vital for anti-HIV-1 activity. Cytotoxicity concentrations (CC50) were reported but its significance was not described.
In short, the above three experiments conducted in the US, Egypt and China respectively making use of different 8-Hydroxyquinoline derivatives including an established drug proved that Hydroxyquinoline possessed the potential as an antiviral and antibacterial agent nonetheless much substantiation on its mode of inhibition, safety and effectiveness are required.
Limitations of the included studies
There are many factors that can influence the validity of the experiments. The reproducibility of the studies would be challenging due to poorly defined negative and positive controls. Lack of consistency in the methodologies in all the studies also makes interpretation and comparison difficult as to determine what is the molecular structure and which compound may actually has the maximum inhibitory potential toward DENV replication. Most studies only used DENV2 assay only and none has been tested on all 4 dengue serotypes. Lai et al (10) mentioned that the primary amino acid sequences of NS2B cofactor and NS3 protease domains of DENV2 and DENV3 revealed overall sequence identity of only ~73%. The lack of data on the cytotoxicity of the compounds were questionable as well thus the safety issue needs more validation prior use to human. The work experimenting on both 8-Hydroxyquinoline and dengue virus is very limited therefore studies concerning West Nile virus and other virus and bacteria were included for review making this paper lack specification.
By focusing on individual articles, in the first study (30), the use of HTS was credential for structure-based design of small molecule inhibitors of proteases, however structure-activity relationship (SAR), WNV infectivity assay and viral protein expression were not performed. The subsequent studies (9, 10) complemented the previous study and showed good reports in favour of 8-HQ scaffold as a potential dengue viral inhibitor, however it could not describe the protease-inhibitor complex orientation.
Amodiaquine promised a better candidate as an antiflaviviral therapy, nevertheless its toxicity level is not well established. More researches are needed to identify the target and exact step that is targeted by AQ in addition to finding derivatives of the drug that are the least cytotoxic for the use in dengue fever patients (31).
The synthesis of new quinoline derivatives via cyclization of 8-Hydroxyquinoline-5-sulphonyl chloride were shown to have some antimicrobial and antiviral activity however the implications of its use lack justification (32).
The study done to find for new anti-HIV-1 agents was rather basic as it was a preliminary study and will require more authentication on its effectiveness and safety level (33).
Recommendation on future work
In the future, further studies are needed to solve the co-crystal structure of the protease-inhibitor complex of DENV in order to gain insight into the exact orientation of the compound in the active site. This knowledge would tremendously help in antiviral drug development. Otherwise, other approaches as listed by Lim et al (24) could be experimented as well.
It is worth noted that a clinical trial using Celgosivir was conducted on 50 dengue patients in Singapore. Celgosivir was a naturally occurring iminosugar derived from the seeds of Castanospermum austral. Though the drug was generally safe and well tolerated, it did not significantly reduce viral load (p value 0.203, 90% CI -0.65 to 0.22) or fever burden in the subject (p value 0.973, 90% CI 2.16 to 26.25) (34). This implies that the effort to find a potential cure for dengue is still a long journey to embark.
CONCLUSION
In conclusion, there were limited references available in order to suggest or dispute the use of 8-Hydroxyquinoline as a potential antidengue agent. The available articles have limitations in many aspects and the results lack implications. Most authors involved in the studies also did not continue their work on the same compound and the same disease.
Though 8-Hydroxyquinoline may be a promising agent, further investigations with a proper methodology and outcomes need to be conducted to yield results that can be translated into in vivo and clinical studies.

REFERENCES
1. WHO. Dengue and severe dengue [Internet]. WHO Fact Sheet. 2012. p. 1–4. Available from: www.who.int/mediacentre/factsheets/fs117/en/index.html
2. Gubler DJ. Dengue and Dengue Hemorrhagic Fever. Clin Microbiol Rev [Internet]. 1998 Jul 1 [cited 2015 Aug 24];11(3):480–96. Available from: http://cmr.asm.org/content/11/3/480.full
3. Murray NEA, Quam MB, Wilder-Smith A. Epidemiology of dengue: past, present and future prospects. Clin Epidemiol [Internet]. 2013 Jan [cited 2015 Feb 5];5:299–309. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3753061&tool=pmcentrez&rendertype=abstract
4. www.dengue.info [Internet]. [cited 2015 Aug 25]. Available from: http://www.dengue.info/
5. Kuno G. Emergence of the severe syndrome and mortality associated with dengue and dengue-like illness: historical records (1890 to 1950) and their compatibility with current hypotheses on the shift of disease manifestation. Clin Microbiol Rev [Internet]. 2009 Apr [cited 2015 Aug 24];22(2):186–201, Table of Contents. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2668235&tool=pmcentrez&rendertype=abstract
6. Hess D. Clinical practice guidelines. Int Anesthesiol Clin. 1996;10.
7. Posts about Dengue on Director General of Health Malaysia [Internet]. [cited 2015 Dec 3]. Available from: http://kpkesihatan.com/category/communicable-disease/dengue/
8. CDC – Epidemiology – Dengue [Internet]. [cited 2015 Aug 24]. Available from: http://www.cdc.gov/dengue/epidemiology/
9. Ezgimen M, Lai H, Mueller NH, Lee K, Cuny G, Ostrov DA, et al. Characterization of the 8-hydroxyquinoline scaffold for inhibitors of West Nile virus serine protease. Antiviral Res [Internet]. 2012 Apr [cited 2015 Aug 21];94(1):18–24. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3331929&tool=pmcentrez&rendertype=abstract
10. Lai H, Sridhar Prasad G, Padmanabhan R. Characterization of 8-hydroxyquinoline derivatives containing aminobenzothiazole as inhibitors of dengue virus type 2 protease in vitro. Antiviral Res [Internet]. 2013 Jan [cited 2015 Aug 21];97(1):74–80. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3568461&tool=pmcentrez&rendertype=abstract
11. Brecher M, Zhang J, Li H. The flavivirus protease as a target for drug discovery. Virol Sin [Internet]. 2013 Dec [cited 2015 Aug 21];28(6):326–36. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3927373&tool=pmcentrez&rendertype=abstract
12. Tropical Plant Database entry for: Quinine Bark (Cinchona) [Internet]. [cited 2015 Aug 24]. Available from: http://www.rain-tree.com/quinine.htm#.VdrnHvmqqkp
13. Globinmed – Cinchona sp. [Internet]. [cited 2015 Aug 21]. Available from: http://globinmed.com/index.php?option=com_content&view=article&id=83210:cinchona-sp&catid=73&Itemid=146
14. Search results — The Plant List [Internet]. [cited 2015 Dec 15]. Available from: http://www.theplantlist.org/tpl1.1/search?q=cinchona
15. Quinine Uses, Benefits & Dosage – Drugs.com Herbal Database [Internet]. [cited 2015 Aug 21]. Available from: http://www.drugs.com/npp/quinine.html
16. Boratyński PJ. Dimeric Cinchona alkaloids. Mol Divers [Internet]. 2015;19(2):385–422. Available from: http://link.springer.com/10.1007/s11030-014-9563-1
17. Collin G, Höke H. Ullmann’s Encyclopedia of Industrial Chemistry [Internet]. Weinheim, Germany: Wiley-VCH Verlag GmbH & Co. KGaA; 2000 [cited 2015 Aug 26]. Available from: http://onlinelibrary.wiley.com/doi/10.1002/14356007.a22_465/full
18. SMITH JN. Studies in detoxication. 53. The glucuronic acid conjugation of hydroxyquinolines and hydroxpyridines in the rabbit. Biochem J [Internet]. 1953 Aug [cited 2015 Aug 26];55(1):156–60. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1269150&tool=pmcentrez&rendertype=abstract
19. Short BRD, Vargas MA, Thomas JC, O’Hanlon S, Enright MC. In vitro activity of a novel compound, the metal ion chelating agent AQ+, against clinical isolates of Staphylococcus aureus. J Antimicrob Chemother [Internet]. 2006 Jan [cited 2015 Aug 26];57(1):104–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16319182
20. Prachayasittikul V, Prachayasittikul S, Ruchirawat S, Prachayasittikul V. 8-Hydroxyquinolines: a review of their metal chelating properties and medicinal applications. Drug Des Devel Ther [Internet]. 2013 Jan [cited 2015 Aug 21];7:1157–78. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3793592&tool=pmcentrez&rendertype=abstract
21. Short BRD, Vargas M a, Thomas JC, O’Hanlon S, Enright MC. In vitro activity of a novel compound, the metal ion chelating agent AQ+, against clinical isolates of Staphylococcus aureus. J Antimicrob Chemother. 2006;57(1):104–9.
22. Moret V, Dereudre-Bosquet N, Clayette P, Laras Y, Pietrancosta N, Rolland A, et al. Synthesis and anti-HIV properties of new hydroxyquinoline-polyamine conjugates on cells infected by HIV-1 LAV and HIV-1 BaL viral strains. Bioorganic Med Chem Lett. 2006;16(23):5988–92.
23. Brinton MA. The molecular biology of West Nile Virus: a new invader of the western hemisphere. Annu Rev Microbiol [Internet]. 2002 Jan [cited 2015 Dec 9];56:371–402. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12142476
24. Lim SP, Wang QY, Noble CG, Chen YL, Dong H, Zou B, et al. Ten years of dengue drug discovery: Progress and prospects. Antiviral Res [Internet]. Elsevier B.V.; 2013;100(2):500–19. Available from: http://dx.doi.org/10.1016/j.antiviral.2013.09.013
25. Libraty DH, Endy TP, Houng H-SH, Green S, Kalayanarooj S, Suntayakorn S, et al. Differing influences of virus burden and immune activation on disease severity in secondary dengue-3 virus infections. J Infect Dis. 2002;185(9):1213–21.
26. De Clercq E. Anti-HIV drugs: 25 compounds approved within 25 years after the discovery of HIV. Int J Antimicrob Agents [Internet]. Elsevier; 2009 Apr 4 [cited 2015 Sep 7];33(4):307–20. Available from: http://www.ijaaonline.com/article/S0924857908004846/fulltext
27. Wyles DL. Antiviral resistance and the future landscape of hepatitis C virus infection therapy. J Infect Dis [Internet]. 2013;207 Suppl(suppl_1):S33–9. Available from: http://jid.oxfordjournals.org/cgi/content/long/207/suppl_1/S33
28. Romano KP, Ali A, Royer WE, Schiffer CA. Drug resistance against HCV NS3/4A inhibitors is defined by the balance of substrate recognition versus inhibitor binding. Proc Natl Acad Sci U S A [Internet]. 2010;107(49):20986–91. Available from: http://www.pnas.org/content/107/49/20986
29. Li J, Lim SP, Beer D, Patel V, Wen D, Tumanut C, et al. Functional profiling of recombinant NS3 proteases from all four serotypes of dengue virus using tetrapeptide and octapeptide substrate libraries. J Biol Chem [Internet]. 2005;280(31):28766–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15932883
30. Mueller NH, Pattabiraman N, Ansarah-Sobrinho C, Viswanathan P, Pierson TC, Padmanabhan R. Identification and biochemical characterization of small-molecule inhibitors of west nile virus serine protease by a high-throughput screen. Antimicrob Agents Chemother. 2008;52(9):3385–93.
31. Boonyasuppayakorn S, Reichert ED, Manzano M, Nagarajan K, Padmanabhan R. Amodiaquine, an antimalarial drug, inhibits dengue virus type 2 replication and infectivity. Antiviral Res [Internet]. 2014 Jun [cited 2015 Aug 21];106:125–34. Available from: http://www.sciencedirect.com/science/article/pii/S0166354214000886
32. Kassem EM, El-Sawy ER, Abd-Alla HI, Mandour AH, Abdel-Mogeed D, El-Safty MM. Synthesis, antimicrobial, and antiviral activities of some new 5-sulphonamido-8-hydroxyquinoline derivatives. Arch Pharm Res [Internet]. 2012 Jun [cited 2015 Dec 11];35(6):955–64. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22870804
33. Zeng X-W, Huang N, Xu H, Yang W-B, Yang L-M, Qu H, et al. Anti human immunodeficiency virus type 1 (HIV-1) agents 4. Discovery of 5,5’-(p-phenylenebisazo)-8-hydroxyquinoline sulfonates as new HIV-1 inhibitors in vitro. Chem Pharm Bull (Tokyo). 2010;58(7):976–9.
34. Low JG, Sung C, Wijaya L, Wei Y, Rathore APS, Watanabe S, et al. Efficacy and safety of celgosivir in patients with dengue fever (CELADEN): a phase 1b, randomised, double-blind, placebo-controlled, proof-of-concept trial. Lancet Infect Dis [Internet]. 2014 Aug [cited 2015 Aug 27];14(8):706–15. Available from: http://www.sciencedirect.com/science/article/pii/S1473309914707303

